When you hear the word "trauma," what first comes to mind?
This word is usually associated with things that are horrible to experience, such as a car accident or the sudden death of a loved one. What follows are emotions like shock or denial because of the event. Your life could have been going along smoothly, and then suddenly something happens that literally turns your world upside down.
Have you ever considered that as a caregiver to a child with special needs, you have experienced trauma, repeatedly, for weeks or months or years on end? Events that have turned your life upside down, have stopped you in your tracks, have caused shock, denial, fear, anger, resentment, or grief?
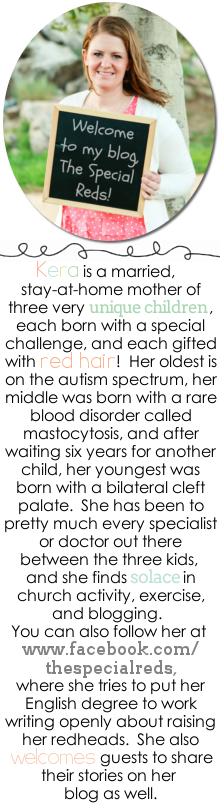
Honestly, it wasn't until I helped to organize a meeting for a local caregiver support group that I realized how much trauma I have experienced as a mom. I went through years of uncertainty trying to figure out my daughter's diagnosis, trying to cope with the fact that her path would be different, trying to get her the right help. Hours upon hours on the phone, going to doctor after doctor, trying diets, evaluations and assessments, dealing with challenging behaviors where I had no idea what to do, grieving over the uncertainty of her future. And then with my second child, I went through the same uncertainty and fear as I sought his medical diagnosis so he could receive the right treatment. And then with my youngest, it was the shock in the hospital, hours after his birth, where we were given his diagnosis, and I knew nothing would be what I imagined for him. These situations I've faced as a mother, if you really look at them, have been traumatic--they have brought me to my knees and kept me from experiencing what some might call a more "normal" motherhood experience.
An article I used for that caregiver meeting explains trauma so well. The author, Eileen Devine, LCSW, shares a story of how one of her clients describes her life that week with her daughter who has behavioral challenges associated with fetal alcohol syndrome. Devine says, "Although the week had been particularly difficult, in reality the last two years, overall, had been incredibly difficult." When I read this, it really struck me--I realized I have been experiencing traumatic event after traumatic event for YEARS. Yes, some weeks were harder than others, and some days, but if you add it all up, it equaled a long stream of traumatic events that, when I actually stop to think about it, can't even believe. How have I even made it through all that I have? Am I really doing okay, or am I just in "survival mode," going day to day but not considering how these traumatic events have really changed me or affected me in some way?
I think the difficulty that caregivers face when it comes to trauma is that once that big event happens--the one that changes things forever, NOTHING EVER SLOWS DOWN. You are suddenly given this new road to take with your child, and you have to keep going somehow. Your child is depending on you to obtain the right treatment, services, school placements, medical care, therapies--the list goes on. When do you ever stop to think about how what you are doing as a caregiver is really affecting you--how these traumatic events are piling up, day after day, year after year?
Devine says, "I don't say this lightly, but in parenting children whose brains work differently, each is separately living through, on a daily basis, a traumatic event. It's no wonder that these parents frequently describe being depressed, anxious, and on-edge. It's no wonder that they might find themselves physically ill much of the time, with ailments that rarely seem to abate or resolve...Many parents are left wondering how they ended up in such a dark place, and how they might ever extract themselves again."
It's important to point out here, that this "place" Devine mentions is actually what she calls "caregiver burnout," which I will discuss in a future post. But I share her thoughts because I want you as caregivers to see how these traumatic events really do add up and can lead to this burnout.
Another important point I want to stress here is the sadness I feel when I consider the fact that the trauma I have experienced in my life has largely been from the health challenges my children have faced. I don't like thinking about it that way--that because of the challenges my children have been given, I now have gone through serious trauma. This negative view is not something I want to adopt as their mother. I think this is why it's crucial that we see our child for who they really are and not just the disability or health concerns--they are our children first. As caregivers, we are tasked with helping our children navigate life as they also deal with the symptoms that come from these diagnoses. This asks a lot more of us as parents, but what parent isn't willing to do everything they can to help their child? Make sure you are seeing your child first and the diagnosis second so you don't fall into anger or resentment, or blaming your child for what you have to go through with them--it's NOT their fault.
I remember the trauma I went through after my youngest had his palate repair surgery. It was the first time any of my children had had surgery, so I was a wreck, to say the least. It was rescheduled twice because of emergency operations that needed to be performed by his surgeon, so we were pushed back by several months already. The day finally came, and it was at a horrible time for all of us--right in the beginning of a new school year. The surgeon didn't give a lot of details about how the surgery was going to happen, and he explained that the recovery was usually just one day in the hospital. I really didn't think it would be too bad, based on what he told me, and based on the fact that I didn't know anyone who had been through this before--all of this was very new to us.
The surgery was longer than he said it would be--my husband and I waited in the hospital with all the other worried parents and families until our son's number moved down the screen. And when we finally got to see him, I nearly broke down. His face was swollen and he had to breathe with a tube. He looked absolutely miserable and I so wished I could take all his pain away. I asked the surgeon more about how the repair was done. He actually drew a picture, showing that he removed both sides of the existing palate in his mouth that never fused together, sewed them together down the middle, then stretched it out to the gum line, inserting stitches all along the gumline. So he had stitches down the middle of his palate and all around the gums. The very thought of my baby going through this made me cringe. But I tried to remain hopeful--he said the hospital stay would only be one night and he would be feeling much better.
Well, that didn't happen--one night turned into three and my little baby still didn't want to eat. When he finally got at least one ounce down from a bottle, the doctors reluctantly sent me home, but told me to watch for signs of dehydration. Those next few weeks were rough getting him to eat, and I came close to bringing him back to the hospital. But we got through it, and with the exception of a small fistula, or hole, in his palate, (which was whole other traumatic experience in itself) he is doing just fine.
Those days in the hospital with him were certainly traumatic. Every time I had to return for follow-up appointments, I had to drive by the hospital. Just the sight of that building triggered horrible, fearful feelings. It took about 2 years before I could drive by it without fear creeping inside of me, taking me back to those long, difficult days trying to get him to eat. Add to this the dozens of other traumatic experiences I've had with him since then and you have a recipe for disaster. Trauma after trauma after trauma, with no time to regroup or "go back to normal." My normal was going to be filled with trauma and there was no escaping it.
Going back to last week's post about accepting our role as caregiver, you could add one more point to the list--accepting the fact that trauma will be a part of your life now. But how can we deal with trauma in a way that won't lead to burnout? Here are some things I think helped me get to where I am now:
1. Talk about what you are experiencing with others--this can be a great support system.
I mentioned the hours I spent on the phone trying to get help or answers for my daughter earlier in this post, and that is no exaggeration. Those hours on the phone weren't just with doctors, teachers, or specialists--they were also with my family and friends, who became a huge support for me during that time. I pretty much talked everyone's ear off during those early years--I was trying to figure things out and process what was happening, and I was lost! Talking openly about my struggles (or what I would now call "traumatic events") with others is really what saved me and gave me the support I needed. If you aren't talking to others about what you are facing on a regular basis, start now! You can't keep all of this inside. Writing about it is another great tool.
2. Don't dwell on the past too much--look at where you are now.
There can be a lot of painful memories associated with being a caregiver--memories that, if you dwell on them for too long, might not allow you to appreciate where you are currently. I did a lot of journaling, and then blogging, back in my earlier days as a mother. When I read those entries, the tears start flowing, but not because I am sad--because I am grateful for how far I've come. I can look back and see what I've been able to get through, and it is empowering to me. It gives me confidence to keep going forward. Maybe you are right in the middle of those traumatic experiences and can't begin to imagine looking back yet--keep going so you can. And even look back on yesterday, or a week ago, and see what has changed. Try to find those little blessings and miracles that got you to where you are.
3. Make sure to take some time for yourself.
Of course this is easier said than done. But it's absolutely essential to dealing with the many traumatic events that caregivers face on a regular basis. For me, in those earlier years, it was exercise. I had to go to the gym or go for a walk every day to feel okay. Figure out what will help you deal with your situation and make it a priority. You are important, too!
The traumas that I face as a caregiver now have calmed down, for the most part, or maybe I have just learned to adjust to my "normal." I continue to talk to people, to write. I continue to look back on what I've been through and realize how far I've come. And I continue to take time for myself--right now, it's pursuing a graduate degree.
Some questions to consider: What traumatic events have you experienced as a caregiver? What has turned your life upside-down? What can you do to deal with traumatic events in a healthy way?
As caregivers, we can't escape the trauma that will come into our lives, but we can view them as stepping stones on our journey as we learn how to care for our children.
Next week I will share my thoughts on a new topic related to caregiving: relational stress.
Link to article by Eileen Devine: Managing the Toll of Caregiver Trauma
Sunday, March 24, 2019
Sunday, March 17, 2019
6 Ways You Can Embrace Your Role as a Caregiver
When I think about all the moments that have defined me as a mother, there is one that stands out above all others. This one moment was a realization I truly needed to move forward and face the challenges I knew were ahead of me.
It was when I was in the hospital, about a day after my youngest son was born. We had already been told about his cleft palate and had met with many doctors to go over what his treatment plan would look like and the next steps to take. We had spent the majority of our time trying to figure out the best way to feed him, and once I saw that he could to suck on a pacifier, we fed a tube syringe with formula through the small hole on the Nuk pacifier and slowly released the formula into his mouth from the syringe. It wasn't true suction because he had no palate, but he was able to imitate sucking as best he could with the pacifier, and he was eating. We were all so relieved to find something that would work for him, and the nurses said I could finally bring him to my room to stay with me.
I got to be with my new baby in my room--just me and him. I got to hold him and love him the way I had wanted to since he was born. Things had been so chaotic since his birth that I hadn't had time to stop and realize what this meant for me as a mom. And it hit me, pretty hard in that moment--I now had three children, each with various needs. My husband and I had spent my entire pregnancy praying that this baby would be healthy and normal, and he wasn't--at least that's how I felt in those early days. We longed to just love a baby with no extra needs--and now here I was, with another baby taking me on a completely new journey as a mom. I knew nothing about cleft palate, about palate repair surgeries, about exclusive pumping, about feeding with special bottles, about how many doctor appointments he would need. I wondered why my Heavenly Father would send me a child with these challenges knowing what we had already been through with our previous children. Could I do this? I fell deep into the "why me" line of thought, and I knew that wasn't the right solution.
I continued to ponder on my reality as I fed my new baby with the tube-syringe method. He took to the method so gracefully--I would say it was a miracle! One of the doctors came in and remarked that he had never seen a mom of a baby with cleft palate learn so quickly to adapt and feel comfortable with feeding. The only words I could reply (and I've written about this here) were, "I'm not really sure. I guess it's because I'm his mom."
As soon as I uttered those words, all the "why me's" vanished. I no longer wondered why our prayers weren't answered, because they were. I knew Heavenly Father gave me this child because He knew I could take care of him--I was prepared because I had gone through challenges with my older children--except this time, I wouldn't have to go through any searching to find answers--they were all given to me before he left the hospital (for the most part.) I left that hospital with a team of people behind me who I knew would help me any time I called--I didn't have that with my first two children. Things were going to be okay. This was the moment that defined me as a mother--I now saw the unique role that I was given because of my children. And though I wouldn't have used this word back then, the word I want to use now to define that role is that of a caregiver.
What is a caregiver? This word isn't always used when referring to a parent of special needs children--more commonly, it's used in reference to caring for an elderly person. But it is exactly what we are--we are caregivers. The best definition of caregiver that I can find comes from the churchofjesuschrist.org. It says:
"A caregiver is a person who provides regular care for someone who is unable to meet some or all of their own needs. Often the person receiving the care is a family member living with a physical or mental disability, chronic illness, or effects of old age. The time commitment required to care for such
individuals may range from a few hours a week to 24-hour care.
Caregivers are often required to balance work, church,
and other family responsibilities while at the same time attempting to provide
individual care to a loved one. While providing care is often a very rewarding
and enriching experience, the demands of continual care can also cause worry,
exhaustion, financial stress, anxiety, and fatigue. Caregivers may have needs
that are not visible to others, and they may also be reluctant to ask for help.
Caregivers may have a higher risk of stress-related depression, anxiety,
substance abuse, or physical health issues. They may also experience grief,
resentment, or anger over the loss of their hopes, expectations, and even
dreams. Their day-to-day lifestyle, freedom to do things they want, and goals
for the future may all be different from what they once expected."
Does this describe your role? Are you caring for someone who cannot meet all of his or her needs? Are you spending a large amount of time caring for this person? Do you find it difficult to balance your role as a caregiver with other aspects of your life? Do you struggle to ask others for help? Do you have stress or anxiety or other health issues? Or do you have anger, grief, or resentment over the loss of your expectation or dreams (of yourself or your child's?) I can certainly answer yes to all those questions.
In those first few days of my youngest child's life, I was able to see clearly what my role was going to be from that point forward. Asking "why" wasn't going to get me anywhere. I love this thought I came across recently from a talk given by M. Joseph Brough: "Frequently, our first reaction to hard things is “Why me?” Asking why, however, never takes away the hard thing." The only way I could help my child in the way he needed me to, and to continue caring for my other children, was to embrace this new role, and embrace it fully.
Now that I can look back on the times I have had to embrace each new role I've been faced with as a mom to my unique children, I can identify what has helped me to accomplish this. That's not to say that there still aren't times that I want to run away and take a long vacation because the pressure can be so intense at times--but even feeling this way, I would never want to change the experiences I've had because they have made me who I am. Here are some ways I have "embraced" being a caregiver.
1. Accept that your child has a health condition or disability.
This was probably one of the hardest things, at least for me. I spent too long in denial over the behaviors my daughter showed in her early years. I just wanted her to be perfect, and I really thought I would never be able to care for her if she wasn't. I wanted things to be easy and more predictable--I wanted to read the normal baby books and follow traditional milestones. I think in some ways, as she grows older and reaches new stages, I find I am having to accept things all over again, and it's hard. But without acceptance, there is no way you can fulfill your role as a caregiver and provide the care needed for your child. Without acceptance, you could find yourself stuck in resentment or anger, which will keep you from loving your child the way he needs to be loved. Acceptance means you are embracing, with open arms, whatever may come.
2. Learn everything you can about your child's disability or health condition.
I think this goes without saying because most parents that I know who have a child with any kind of disability or health condition become experts in that condition--so much that they sometimes know more than doctors! I remember when my neighbor told me she thought my daughter had autism (which I wrote about here). After she left, I cried, for a long time, because, let's be honest--I was scared. But then I went straight to the internet to learn everything I could about autism, and it was the first time I took steps to embrace the role I would have once she received her initial diagnoses. Learning about the health challenges of your child means you aren't afraid--you are arming yourself with knowledge, and this means you are willing to do whatever it takes to care for your child.
3. Don't compare your child to others.
Comparing your child to others is never good, especially when you have a child with a disability or health condition. Celebrate the milestones--big and small--and on your child's timetable only. Throw away the normal baby books! Keep working with your child--follow the advice of doctors, therapists, and don't give up--you will see progress. And when you find yourself in a conversation with other parents bragging about what their child can do, praise your child for what he can do as well, even if it doesn't match up. Doing this will give you more confidence in your role as a caregiver and help you to embrace it for what it is.
4. Be willing to acknowledge that your life will be different now.
When your child receives a diagnosis, you are suddenly thrust on a new path, and, like the definition of "caregiver" mentioned above, you often have to let go of the hopes and dreams that you might have had for your child. Now I want to be clear--this does not mean that you can't set goals for your child, or work hard to help your child reach her potential! It just means you will have to reframe them in a way that is individualized to your own child's strengths and needs, and that's okay. Once you accept this fact, you can more fully embrace your role as a caregiver. In a former article I wrote for The Mighty, I said, "As special needs parents [and I would change this to "caregivers" now], we have to be open to the 'road not taken.' The 'road less traveled' might be a little more lonely, but I can promise you will make new friends along the way."
5. Do your best to stay positive.
This will do wonders for you! I know it's so hard to keep a positive outlook when the days are long and the days turn into weeks and months and years and you feel like there is no end in sight, but there is! It's all about perspective. Some words from a very wise man, Neal A. Maxwell, who suffered from leukemia: "glimpses of eternity can help us to travel the next 100 yards, which may be very difficult.” The way I see it, you can either take the bitter road or the better road. Which one is going to help you be the best caregiver for your child? Which one is going to help you embrace the role that you are in and help your child reach his full potential, whatever that may be? Yes, those next 100 yards may be difficult, but do it with an eternal perspective in mind, and realize that what you are actually doing is serving your child in a way that no one else can--your child needs you.
6. Don't think you have to do all of this in one day.
I decided to add this last step because, let's be real--no one is going to wake up tomorrow feeling like they've accomplished all of these things--it takes time. It's normal to go through stages after your life changes so drastically. I certainly did! I know for a fact that if I hadn't been through the challenges with my two older children, that when my youngest was born with his own challenges I would have completely fallen apart! And you know, I still do sometimes, and that's okay. What matters is that we keep going because we know our kids depend on us.
That day in the hospital was a turning point for me as a mother--the newfound courage that somehow made its way inside me as I uttered those words to the doctor, "I guess it's because I'm his mom," gave me the confidence to move forward in my role as a caregiver. I knew that I had the skills to care for my children, and if I didn't, I would be able to find the answers--and I have. Every step of the way I have been guided as I've been a caregiver to my children.
Maybe you are still struggling with denial, or anger, or sadness. That's okay. You will know when you've reached that turning point and have fully embraced this role as a caregiver to your child.
In the coming weeks, I want to share my thoughts about 4 other topics related to being a caregiver that I have researched for a caregiver support group in our local area: they are trauma, relational stress, compassion fatigue, and caregiver burnout. I will discuss each of these, one at a time, to give more insight into how I've dealt with these in my experience as a mother. I hope you will join me so we can learn together!
Thursday, March 14, 2019
Article for ACPA about Nathan: "Purpose Behind the Cleft"
Has it really been over 2 years since I've blogged on here? Wow, being in college again really makes writing a challenge. I thought I would share a recent article I wrote for the ACPA, which is the American Cleft Palate-Craniofacial Association. It was really well received on their site, and I'm so glad I got the opportunity to share my story and spread awareness about cleft palate, and how it has led me to pursue speech and language pathology. Here's the link to their site Purpose Behind the Cleft, and I have posted the article in its entirety below.
 Our son Nathan was born full term, but he couldn’t nurse and had mucous discharge coming out of his mouth and nose. The nurses took him away for observation, and I sat with my husband in the cold hospital room, listening to the heart monitors beeping, wondering what could possibly be going on. Hours later, the nurses returned to tell us the news: our baby was born with a complete bilateral cleft palate. I knew nothing about clefts, other than that it was a facial difference and that I had seen commercials about it.
Our son Nathan was born full term, but he couldn’t nurse and had mucous discharge coming out of his mouth and nose. The nurses took him away for observation, and I sat with my husband in the cold hospital room, listening to the heart monitors beeping, wondering what could possibly be going on. Hours later, the nurses returned to tell us the news: our baby was born with a complete bilateral cleft palate. I knew nothing about clefts, other than that it was a facial difference and that I had seen commercials about it.
 Our team at Loma Linda University was there for me whenever I had a question, and they made sure Nathan got the best care possible. Nathan began speech therapy at 18 months old to correct articulation and catch up on language development. I got to sit in on his weekly sessions, amazed at the progress he made. Speech therapy seemed like magic to me! I started thinking about going back to school, and I looked into speech therapy. I was lucky enough to finish a 2nd bachelor’s program in communicative disorders at Utah State University and then receive acceptance to a master’s program in speech and language pathology at Idaho State University, where I just finished my first semester.
Our team at Loma Linda University was there for me whenever I had a question, and they made sure Nathan got the best care possible. Nathan began speech therapy at 18 months old to correct articulation and catch up on language development. I got to sit in on his weekly sessions, amazed at the progress he made. Speech therapy seemed like magic to me! I started thinking about going back to school, and I looked into speech therapy. I was lucky enough to finish a 2nd bachelor’s program in communicative disorders at Utah State University and then receive acceptance to a master’s program in speech and language pathology at Idaho State University, where I just finished my first semester.
A little over 6 years ago, my life as a mom changed forever. Our two older children each had their own medical conditions that put us to the test, and we were hoping for a healthy, normal baby throughout my third pregnancy.
 Our son Nathan was born full term, but he couldn’t nurse and had mucous discharge coming out of his mouth and nose. The nurses took him away for observation, and I sat with my husband in the cold hospital room, listening to the heart monitors beeping, wondering what could possibly be going on. Hours later, the nurses returned to tell us the news: our baby was born with a complete bilateral cleft palate. I knew nothing about clefts, other than that it was a facial difference and that I had seen commercials about it.
Our son Nathan was born full term, but he couldn’t nurse and had mucous discharge coming out of his mouth and nose. The nurses took him away for observation, and I sat with my husband in the cold hospital room, listening to the heart monitors beeping, wondering what could possibly be going on. Hours later, the nurses returned to tell us the news: our baby was born with a complete bilateral cleft palate. I knew nothing about clefts, other than that it was a facial difference and that I had seen commercials about it.
Before we knew it, we were being taken to the NICU. A whole team of doctors had arrived to run tests and ask me questions. One of the nurses wanted to show me his cleft palate. I was scared to look. She opened his tiny mouth as far as she could, and I saw it–a huge hole in the top of his mouth. They explained that he would need surgery to correct his palate before he turned one. I felt comforted by the team of doctors and professionals supporting us from the beginning. I knew we wouldn’t be doing it alone, even though we were venturing into unknown territory.
Nathan saw doctors and specialists on a weekly basis at the ACPA Approved Team at Loma Linda University Health group–a plastic surgeon, ENT, and the entire craniofacial team. The speech therapist and nurses helped me through those early months and made sure he was developing normally. Genetic testing was done, and it was discovered that he had a small duplication of chromosome 22, which was very rare, and which likely caused the cleft palate. He had the palate repair surgery at 9 months old, and after the surgery he developed a fistula, or small hole, in the opening of his palate. I was terrified that we’d have to do the surgery again, but the plastic surgeon recommended waiting to see if it would close on its own. I am proud to report that as of today, it is a VERY small hole, which Nathan really likes – it allows him to make his special “clicking” sound.
 Our team at Loma Linda University was there for me whenever I had a question, and they made sure Nathan got the best care possible. Nathan began speech therapy at 18 months old to correct articulation and catch up on language development. I got to sit in on his weekly sessions, amazed at the progress he made. Speech therapy seemed like magic to me! I started thinking about going back to school, and I looked into speech therapy. I was lucky enough to finish a 2nd bachelor’s program in communicative disorders at Utah State University and then receive acceptance to a master’s program in speech and language pathology at Idaho State University, where I just finished my first semester.
Our team at Loma Linda University was there for me whenever I had a question, and they made sure Nathan got the best care possible. Nathan began speech therapy at 18 months old to correct articulation and catch up on language development. I got to sit in on his weekly sessions, amazed at the progress he made. Speech therapy seemed like magic to me! I started thinking about going back to school, and I looked into speech therapy. I was lucky enough to finish a 2nd bachelor’s program in communicative disorders at Utah State University and then receive acceptance to a master’s program in speech and language pathology at Idaho State University, where I just finished my first semester.
Now that I look back on the early years with Nathan, I can see purpose in everything. Yes, we wanted a healthy, normal baby, but you know what? He was healthy, and he is normal. If it weren’t for Nathan’s cleft palate, I would never have been able to sit in on speech therapy sessions and see how wonderful that profession is. I can’t wait to give back to other children when I graduate–to give back to children who are like my Nathan.
Subscribe to:
Posts (Atom)